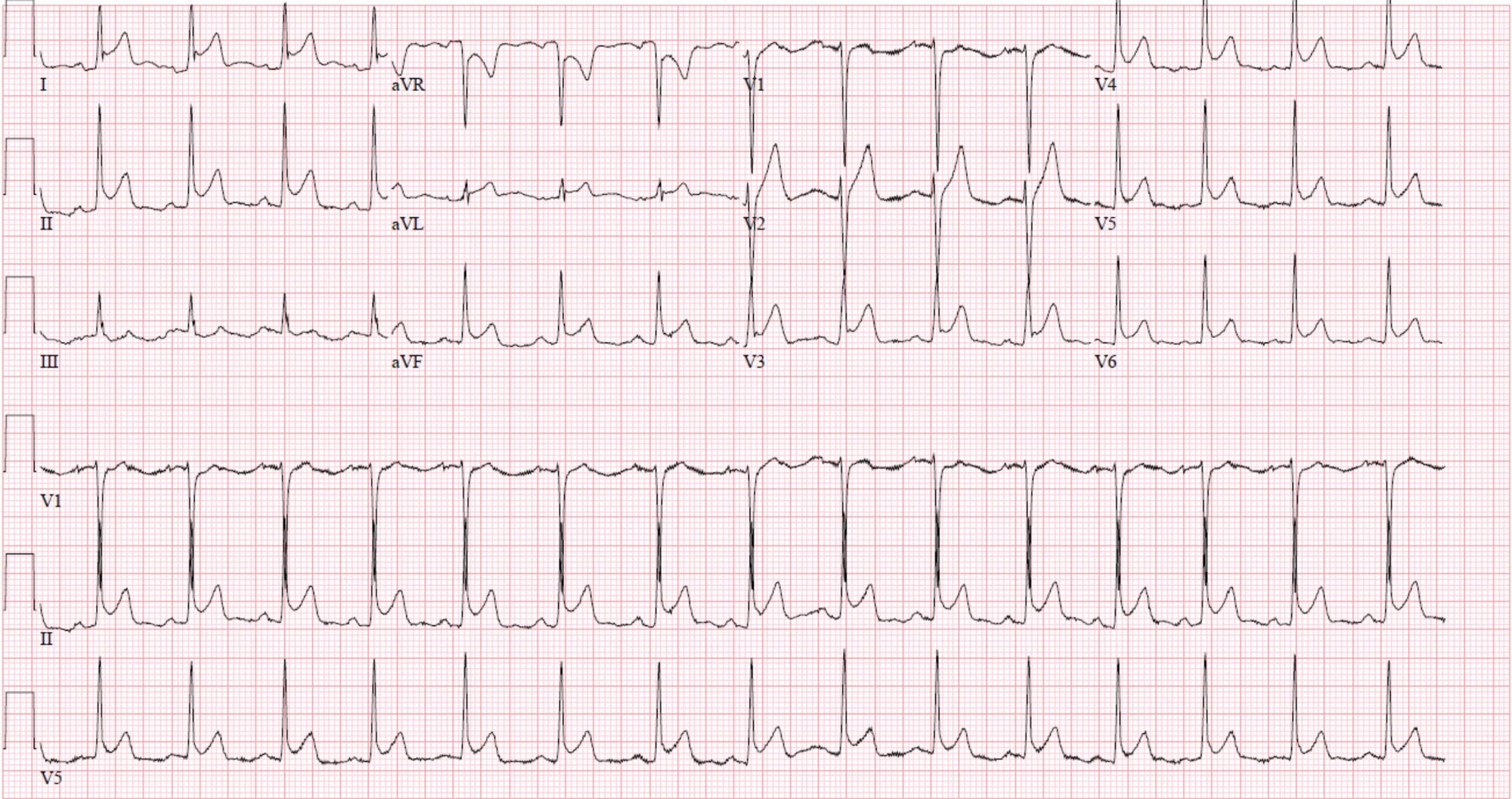
A 37-year-old female presents with sharp, pleuritic chest pain.
What features differentiate acute pericarditis from ST-elevation myocardial infarction? What are the criteria for diagnosing acute pericarditis? What are the treatment options?
Watch Video Summary
What features differentiate acute pericarditis from ST-elevation myocardial infarction?
Differentiating pericarditis from ST-elevation myocardial infarction (STEMI) can be challenging but features that suggest pericarditis over STEMI include any of the following: diffuse concave up ST elevations without reciprocal changes, PR depression, PR elevation in aVR, ST-elevation in lead II greater than lead III, and Spodick’s sign – down-sloping of the TP segment. It is important to note that the test characteristics of any single electrocardiographic feature is insufficient to rule in/out pericarditis, and that the feature with the highest odds ratio for predicting STEMI is reciprocal ST-depressions (Figure 1).
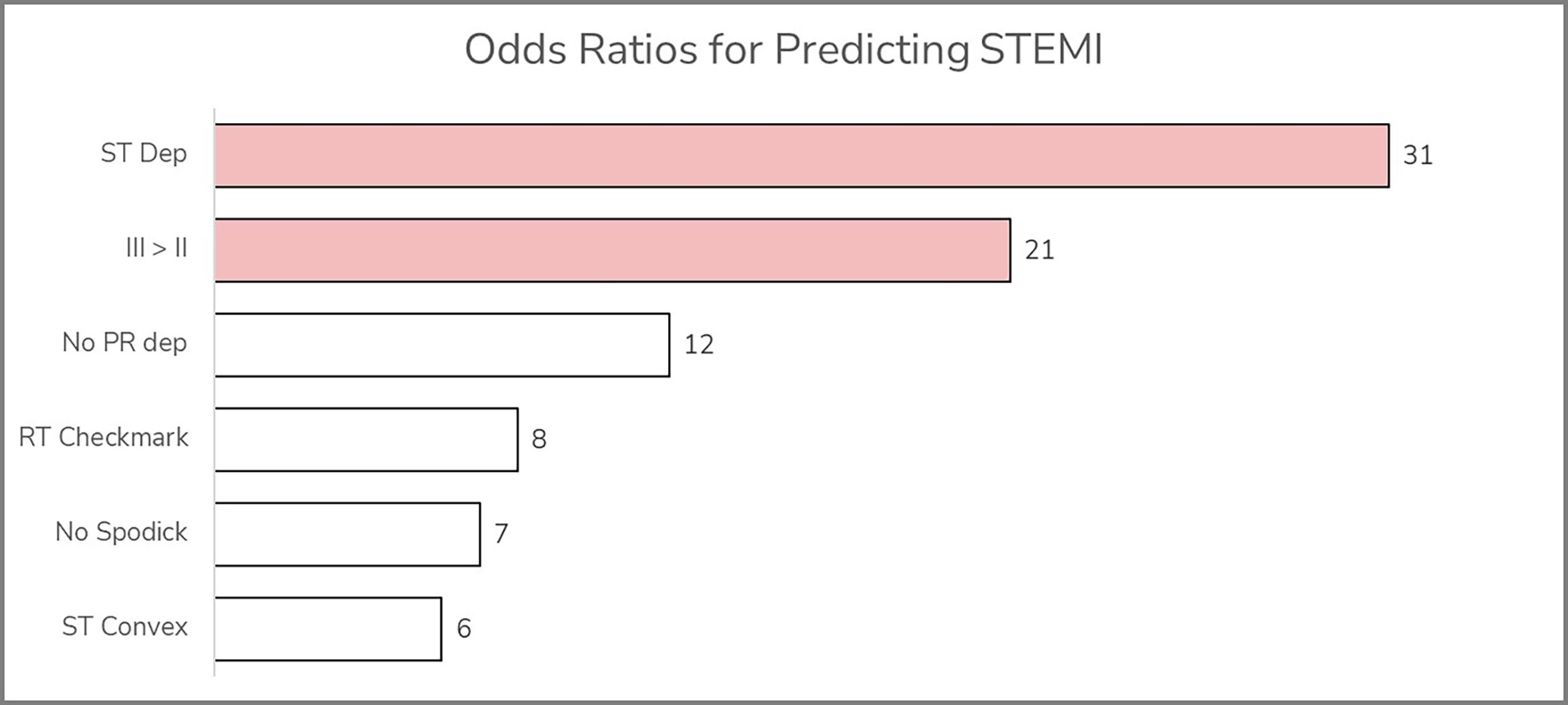
Figure 1. Odds ratios of various ECG findings for predicting STEMI vs. pericarditis. Reciprocal ST depressions (ST dep) and ST-elevation in III>II are the strongest predictors of STEMI.1
The first two weeks are characterized by the above findings. Over several weeks, the ST elevation resolves, and the T waves flatten. Next the T waves invert. Finally, over several weeks the ECG returns to the patient’s baseline (Figure 2).
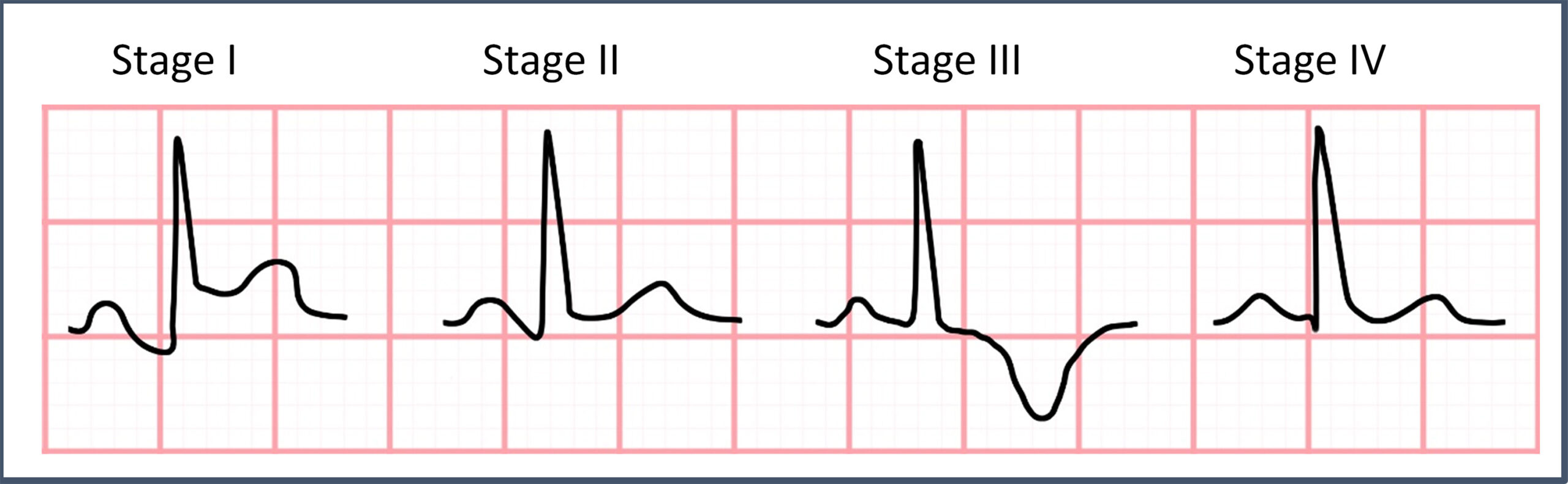
Figure 2. Morphologic features of the various stages of pericarditis.
What are the criteria for diagnosing acute pericarditis?
The diagnosis is made by meeting 2 of 4 criteria2,3:
- Typical symptoms (pleuritic sharp chest pain better when leaning forward)
- New pericardial effusion
- Presence of friction rub
- Typical ECG findings
What are the treatment options?
Colchicine for 3 months and NSAIDs/aspirin tapered over 3-4 weeks are first line in patients without contraindications.4 It’s reasonable to prescribe a proton pump inhibitor also. Corticosteroids are reserved for patients with colchicine/NSAID/aspirin contraindication and are not preferred as they are associated with increased recurrence.3
Pearls for Urgent Care Management
- Electrocardiographic features of acute pericarditis include diffuse concave up ST elevations without reciprocal changes, PR depression, PR elevation in aVR, ST-elevation in lead II greater than lead III, and Spodick’s sign – down-sloping of the TP segment.
- Treatment includes 3 months of colchicine and NSAIDs tapered over 3-4 weeks.
- Uncomplicated, stable patients with acute pericarditis do not need to be transferred to a higher level of care and can be managed in the outpatient setting.
- If the diagnosis is in question, or there are complicating features (e.g., instability), transfer to a higher level of care is appropriate.
References
- Witting MD, Hu KM, Westreich AA, Tewelde S, Farzad A, Mattu A. Evaluation of Spodick’s Sign and Other Electrocardiographic Findings as Indicators of STEMI and Pericarditis. The Journal of Emergency Medicine. Published online March 2020. doi:10.1016/j.jemermed.2020.01.017
- Wagner GS, Strauss DG. Marriott’s Practical Electrocardiography. 12th ed. Lippincott Williams & Wilkins; 2014.
- LeWinter MM. Acute Pericarditis. New England Journal of Medicine. 2017;371(25):349-359. doi:10.1016/j.pcad.2016.12.001
- Imazio M, Brucato A, Cemin R, et al. A Randomized Trial of Colchicine for Acute Pericarditis. New England Journal of Medicine. 2013;369(16):1522-1528. doi:10.1056/NEJMoa1208536

