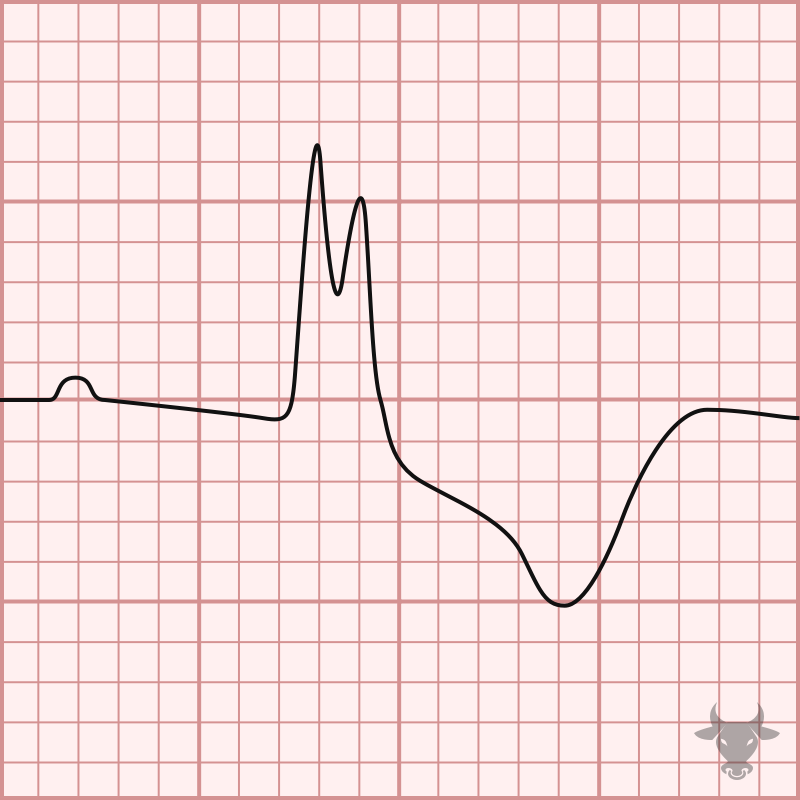
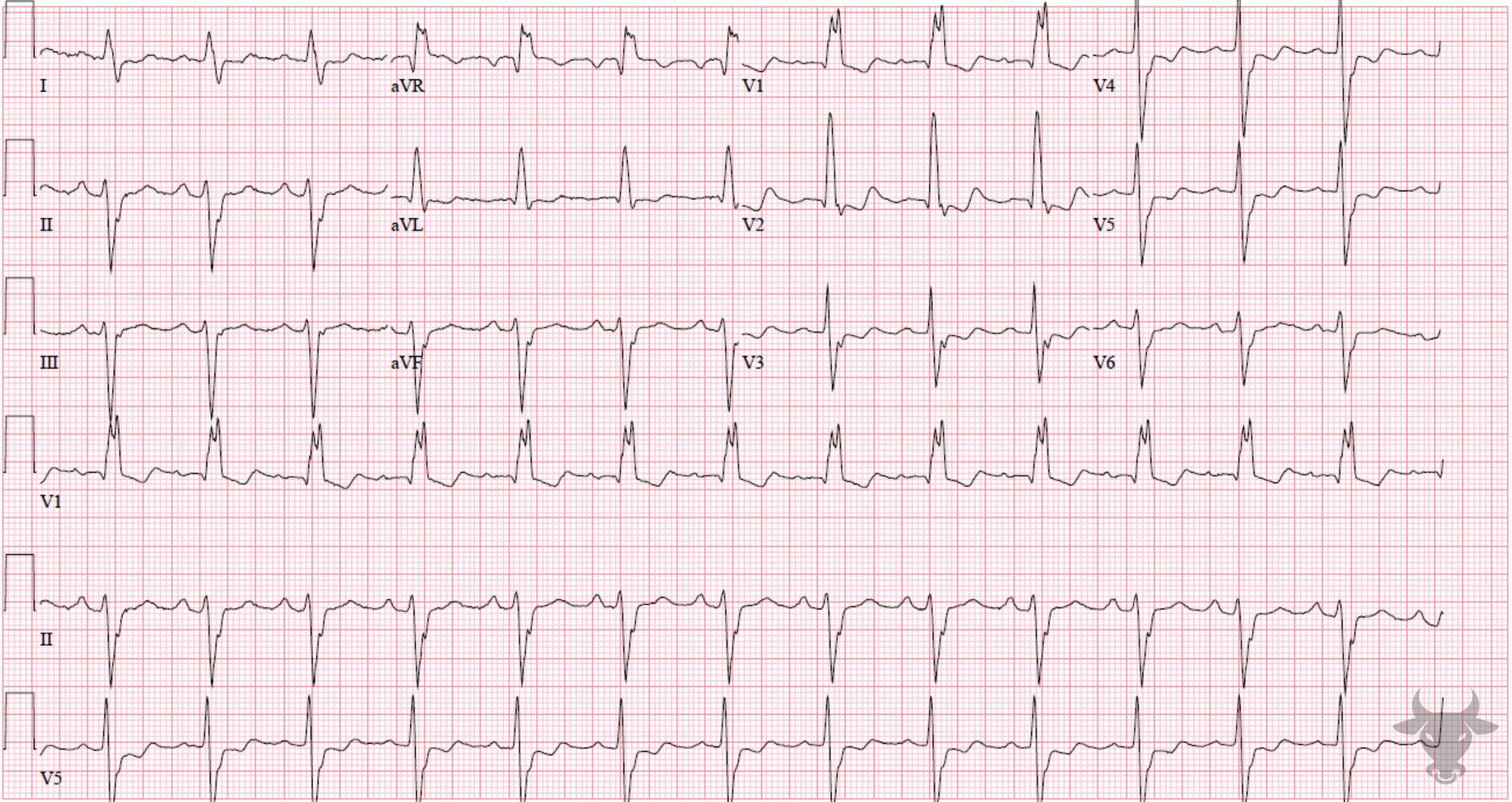
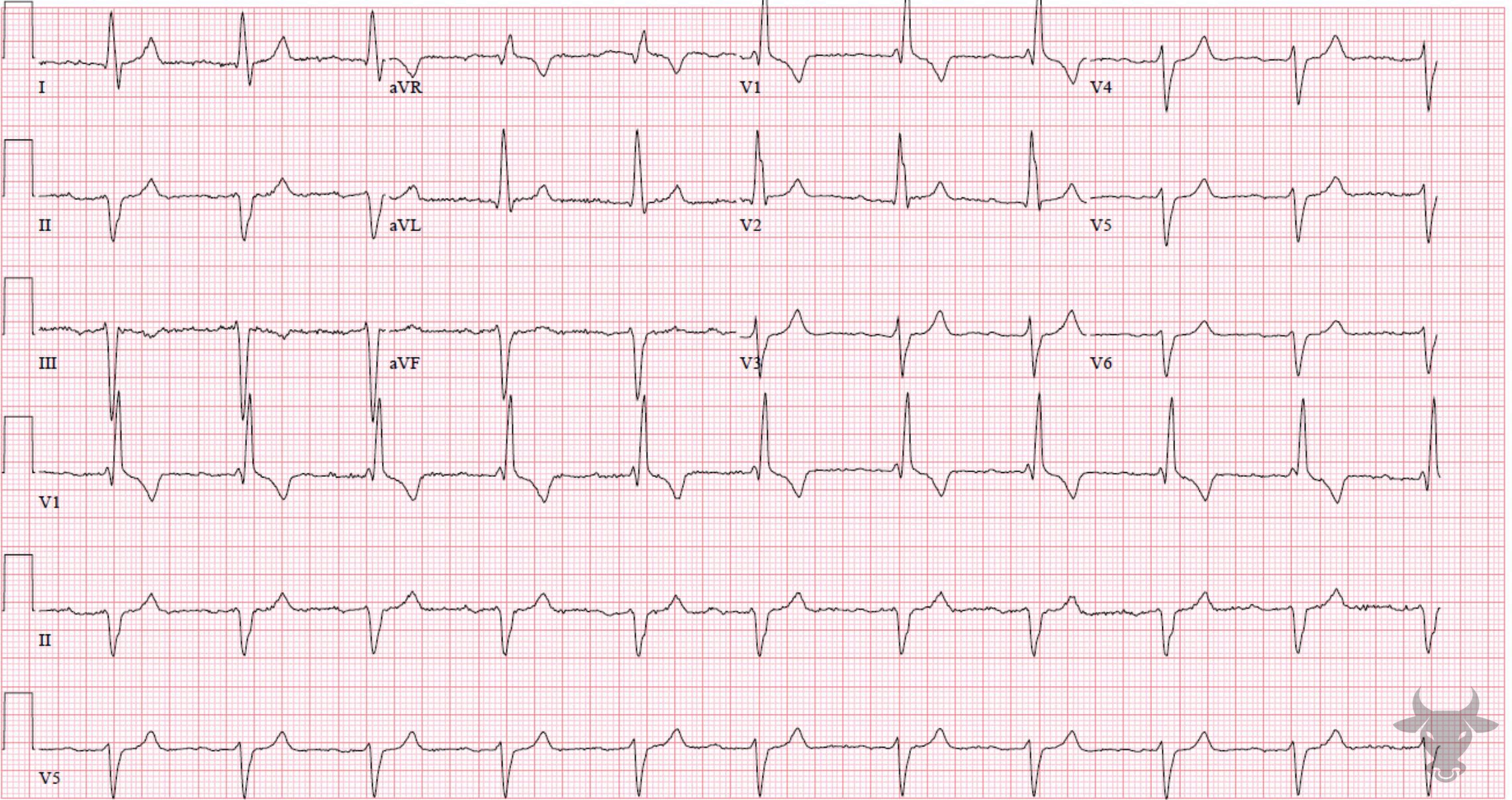
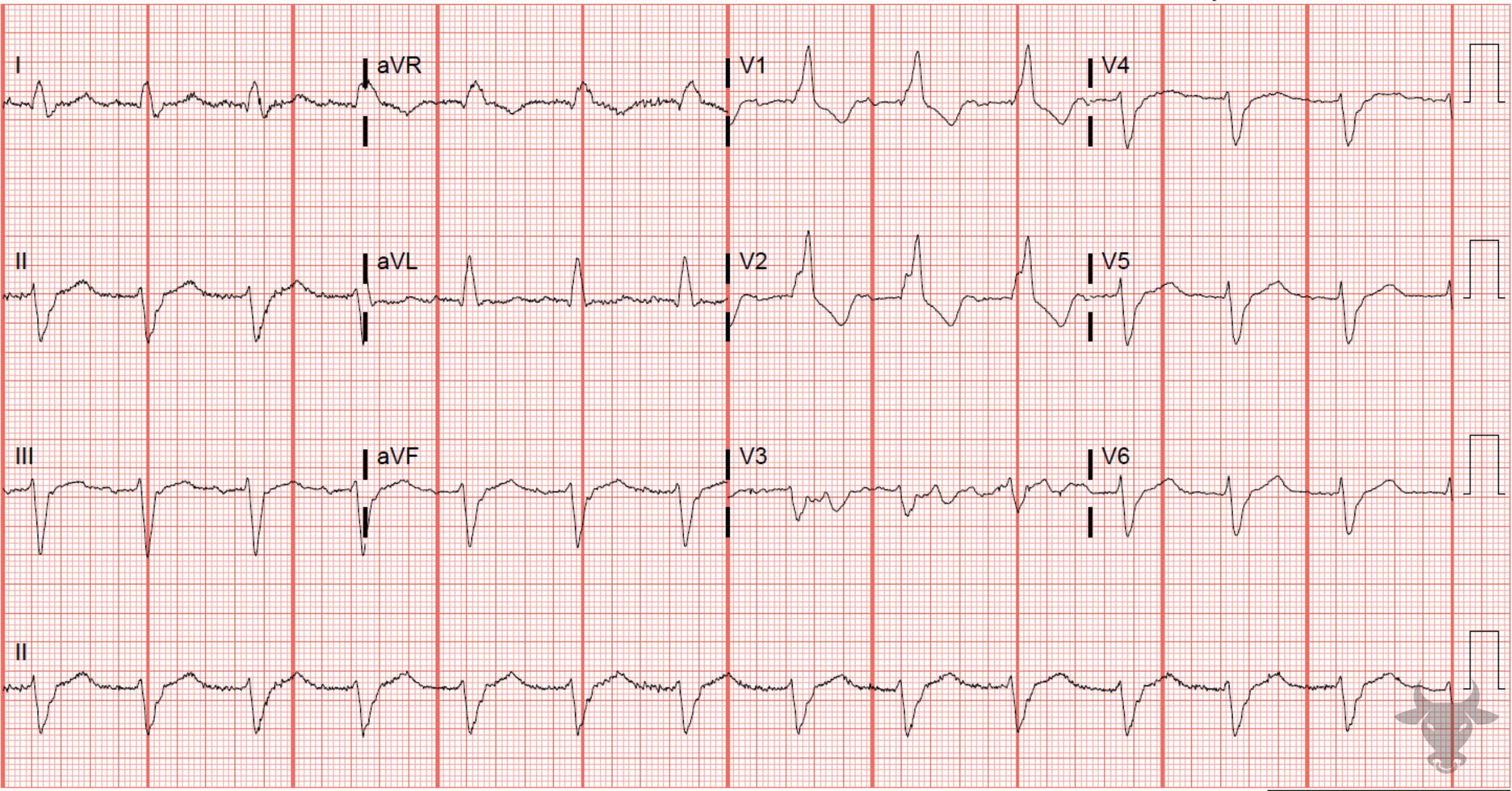
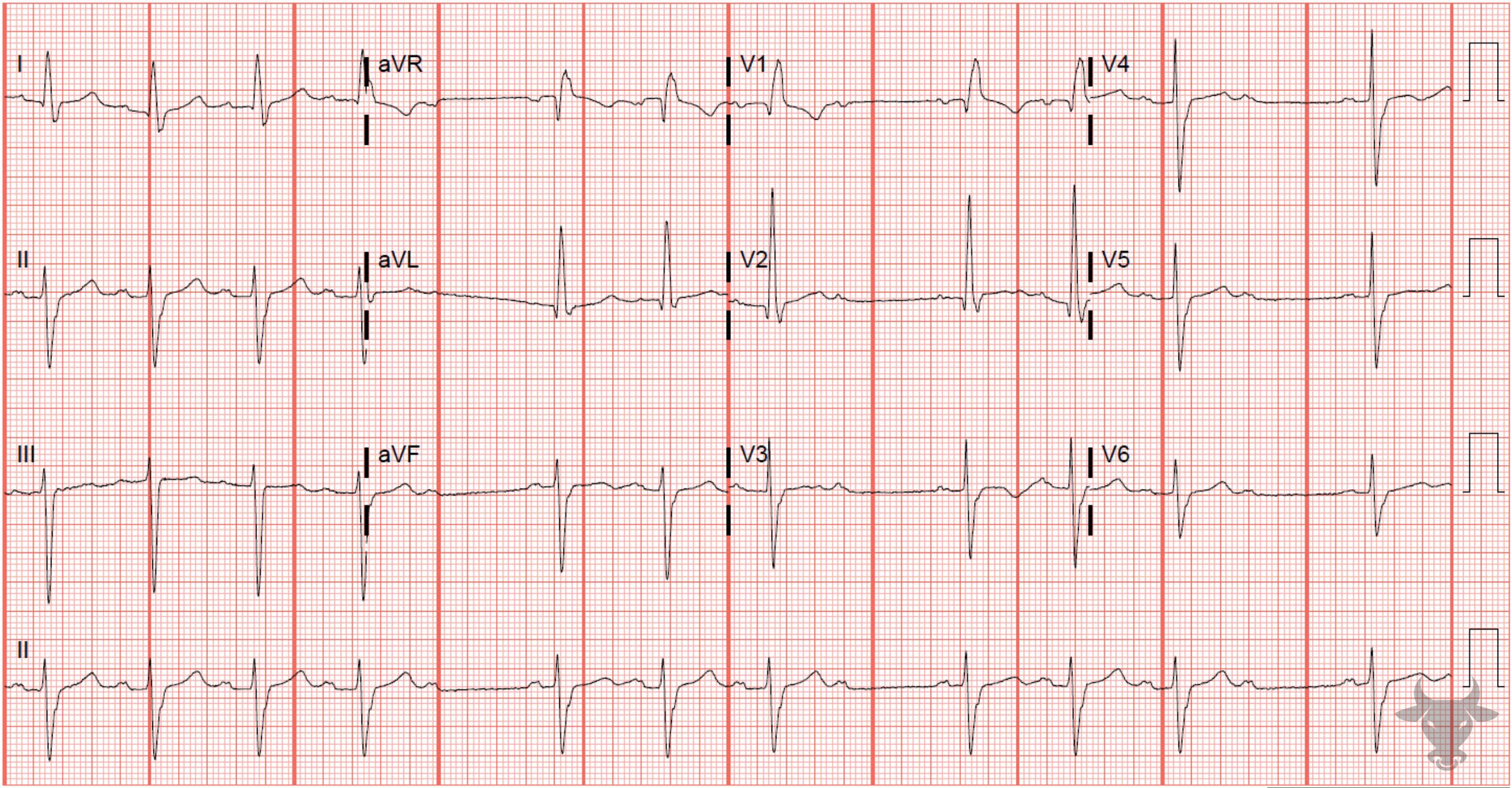
The term “trifascicular block” is a misnomer as a true block of all three fascicles (the right bundle branch, left anterior fascicle and left posterior fascicle) would result in complete heart block. Instead, the term references the presence of diseased conduction in all three fascicles with sufficient sparing of one fascicle (most commonly the left posterior fascicle) that results in delayed conduction and manifests as a prolonged PR interval (1st degree atrioventricular block). The American Heart Association guidelines suggest that use of the term “trifascicular block” be abandoned in favor of a description of the identified blocks independently (e.g. right bundle branch block, left anterior fascicular block, first degree AV-block).
First degree blocks are usually seen it active, healthy patients without heart disease. It usually represents a process within the atrioventricular node itself and is unlikely to progress to complete heart block. However, when accompanied by preexisting conduction disease (e.g. right bundle branch block, left bundle branch block, or bifascicular block) it can indicate infranodal conduction disease. Immediate referral to the emergency department is warranted when patients with significant conduction disease present with symptoms suggesting intermittent bradycardia (e.g. syncope or pre-syncopal lightheadedness) as progression to higher degree blocks including complete heart block should be suspected. These patients should be evaluated for permanent pacemaker placement. The rate of progression to complete heart block in patients with multiple fascicle disease is approximately 1% per year.